One new virus that has cropped up in parts of America could ‘threaten all mankind’ according to experts who predicted the rise of COVID-19, as its related to another virus with a 70% mortality rate in humans.
After the nightmare everyone suffered during the COVID-19 pandemic the last thing anybody wants is to be thrown into the chaos once again, yet the rise of a virus in parts of the US does have some scientists and experts worried.
Earlier in the year similar fears resurfaced surrounding the rise in HMPV cases, as while the bug has been known about for a while, an increase in patients suffering from the virus caused concern in some parts of the world, as the symptoms were similar to that of COVID.
A close relative of the Nipah and Hendra viruses has been detected in parts of North America though, particularly within shrews in Alabama, and those aforementioned viruses are extremely deadly when contracted in humans.


The Camp Hill virus was first spotted within the organs of shrews (DeAgostini/Getty Images)
It’s indicated that they have death rate of around 70%, with symptoms such as a fever, muscle pain, and vomiting alongside more extreme side effects like severe respiratory distress, seizures, and acute encephalitis.
The new discovery has been named the ‘Camp Hill virus’, and was spotted after the frozen organs of shrews captured in 2021 were studied by scientists. It remains a significant discovery as it’s the first time a henipavirus has been discovered in the US, and has raised concerns that similar types could be more common than previously thought.
While it could potentially spread to humans through direct contact with infected animals, Rhys Parry, the lead author of the study that uncovered the Camp Hill virus, has indicated that we shouldn’t jump to conclusions, as reported by Live Science.
“There is no evidence to suggest that the provisionally named Camp Hill virus has infected humans, and the likelihood of it doing so remains unknown but is likely low,” outlined Parry.
The main study advises against a panic, despite the high mortality rate of its relatives like the Nipah virus (Kateryna Kon/Science Photo Library via Getty Images)
As per SurreyLive, that hasn’t stopped leading voices in the field from expressing their own concerns though, as Dr David Dyjack, a specialist from the National Environment Health Association argues:
“What concerns us in public health is that we have this virus with a very high mortality rate, and if it were to mutate and transmit to a human, and attack the kidneys, as we’ve seen in some animals, that could be particularly threatening to all of mankind.”
Dyjack added: “For something like this, if it’s airborne, that causes me great distress as a public health professional.”
Hopefully the Camp Hill virus won’t be even a fraction of how dangerous COVID was for humans, but it’s understandable why many within the field of public health want to get ahead of the curve and act with more caution than perhaps is warranted.
Featured Image Credit: Justin Paget / Getty


A new breakthrough might have been achieved surrounding research into Alzheimer’s disease, indicating that the cause might actually be routed through an infection inside of your mouth.
The disease, thought to be caused by the abnormal build-up of proteins in your brain cells, has largely been considered somewhat of a mystery in medical fields, with no concrete understanding of where it comes from or what it’s caused by.
According to the NHS, factors such as your age, family history, head injuries, and illnesses such as Down’s syndrome and cardiovascular diseases all are linked to the development of Alzheimer’s, but a new scientific study has suggested that a primary cause could be found within your mouth.


Pathogens linked with gum disease have been found in the brains of deceased Alzheimer’s patients (BSIP/Universal Images Group via Getty Images)
As reported by Science Alert, a paper led by Jan Potempa of the University of Louisville has discovered that porphyromonas gingivalis has been found within the brains of deceased Alzheimer’s patients – and that pathogen causes chronic periodontitis, otherwise known as gum disease.
Experiments involving mice corroborated this hypothesis further, as oral infection of porphyromonas gingivalis led to the increased production of amyloid beta, which are the aforementioned proteins that likely cause Alzheimer’s to develop in and around your brain cells.
What, critically, was also discovered was evidence of ‘toxic enzymes’ known as gingipains, which appear to be common in the brains of those affected by Alzheimer’s. This then led to the discovery of gingipains in the brains of deceased individuals who had otherwise never been diagnosed with Alzheimer’s, indicating signals of onset development prior to their passing.
“Our identification of gingipain antigens in the brains of individuals with AD [Alzheimer’s disease] and also with AD pathology but no diagnosis of dementia argues that brain infection with P. gingivalis is not a result of poor dental care following the onset of dementia or a consequence of the late-stage disease,” explains the paper, “but is an early event that can explain the pathology found in middle-aged individuals before cognitive decline.”
This could be the beginning of research that could uncover not only the root causes of Alzheimer’s as a disease – or perhaps an infection – and also enhance preventative treatment once we understand how exactly it activates within the brain.


Studies surrounding P. gingivalis and gingipains could lead to treatment for the disease by reducing baterial load in your brain (Matthew Horwood/Getty Images)
On top of this, the study outlines how small-molecule inhibitor targeting gingipains “reduced the bacterial load of an established P. gingivalis brain infection, blocked [amyloid beta] production, reduced neuroinflammation, and reduced neurons in the hippocampus.
“These data suggest that gingipain inhibitors could be valuable for treating P. gingivalis brain colonization and neurodegeneration in Alzheimer’s disease,” and could then provide a route towards a ‘cure’ of sorts for existing patients and those exhibiting signs of developing the disease.
Featured Image Credit: Peter Dazeley / Getty


Staying on top of HMPV is crucial at a time when the virus is at it’s most dangerous, so understanding the symptoms – specially how they differ from the flu – are essential in order to combat the outbreak.
While it’s hard not to immediately worry that another global pandemic and subsequent lockdown is on the way, thanks to everything we know about human metapneumovirus – otherwise known as HMPV – it’s not likely to cause any major widespread issues.
Doctors have been aware of the virus since 2001, and most people catch it before the age of 5 and continue to encounter it throughout their life, but it’s had a bit of a boost this year particularly due to reports in China that many are calling an outbreak.


A recent uptick in HMPV cases has many considering the situation to be an outbreak of the virus (Idrees Mohammed/AFP via Getty Images)
One of the most dangerous aspects of HMPV though is how easily it’s mistaken for the flu, as at face value many people can’t distinguish the difference when they have it. However, it does have a number of key differences that you can use to identify the virus and hopefully that’ll help everyone stay safe and healthy in the long run.
What’s the difference between HMPV and the flu?
While HMPV’s main symptoms of coughing, nasal congestion, and shortness of breath might initially sound identical to that of the flu, they’re actually far more similar to – albeit more aggressive than – the common cold.
HMPV targets the upper respiratory areas, and can cause bronchitis and potentially even pneumonia in the most severe cases, but the flu is far more likely to affect the entire body.
“Flu typically causes chills, a fever, headaches, muscle aches, and pains,” explains Processor Ron Eccles, as reported by the Daily Mail, continuing on to outline that “the flu feels worse because the symptoms affect the whole body and are not restricted to the upper airways.”
Make sure to take note as to where you’re experiencing the illness, as if it’s just around your lungs and breathing then you might have HMPV as opposed to the flu.


Coughing is one of the most common symptoms of HMPV, whereas full-body chills is more common with the flu (Andreas Rentz/Getty Images)
Thankfully for most people it’s not something you have to worry about too much, as it’s far less dangerous once you’ve already had it, which as previously stated most already have.
Anyone who is immunocompromised, elderly, or young enough to have not caught it yet should exercise caution though, as it can be far more dangerous that a common cold, despite sharing many of the same symptoms.
Your best bet is to practice extensive hygiene measures – which you’re likely already doing – and ensuring that you’re wearing a mask wherever possible.
Featured Image Credit: pocketlight / Hiraman / Getty


Want to live a longer, healthier life?
It turns out, we might learn a thing or two from people living far off the beaten path.
While we all know that eating well, staying active, and avoiding smoking are key to good health, there’s a group of people in the Bolivian jungle who might have even more to teach us.
Scientists claim an indigenous tribe in the heart of the Bolivian jungle are the healthiest humans ever studied.
The Tsimane community is one of the last groups on planet Earth to live a lifestyle focused on hunting, foraging and farming.
They spend less than 10% of their daylight hours in sedentary activities, compared to 54% for people in industralised populations.


Ricardo Lima / MASTER / Getty
Moreover, they have little access to processed foods, alcohol and cigarettes which has major benefits for their health.
Their longevity and remarkable heart and brain health have long amazed scientists.
They have yet to find a single case of Alzheimer’s among the tribe’s 16,000 members, rooted deep in the Amazon rainforest.
Studies also show elderly members of the group have 70% less brain atrophy than those of the same age in more developed countries.
‘We found zero cases of Alzheimer’s among the entire adult population – it is remarkable,’ Bolivian doctor Daniel Eid Rodríguez, a medical coordinator for the researchers, told the BBC.
For over 20 years, anthropologist Hillard Kaplan from the University of New Mexico and his team have studied the Tsimane.
They found the Tsimanes stayed active by hunting animals, planting food and weaving roofs – a typical hunt lasts over 8 hours and covers 11 miles.
The diet especially is different to that of Westerners.


Ricardo Lima / MASTER / Getty
Only 14% of the calories they consume are from fat, compared to 34% in the US, according to the research cited by the BBC.
Their diets are also high in fibre and 72% of their calories come from carbohydrates, whereas in the US it’s 52%.
Additionally, their protein mainly comes from hunted animals like birds, monkeys and fish.
Such lifestyle habits could be the key to longer living in Western societies, scientists have concluded and something we could apply to our own lives.
One challenge with the research is that the Tsimane don’t keep track of their ages very well, so scientists often use the ages of their children to estimate their own ages.
‘Now the most difficult thing is my body. I don’t walk far any more… it will be two days at most,’ a 78-year-old Tsimane called Juan told the BBC.
Despite their impressive health, the Tsimane still face a low life expectancy due to environmental threats.
Featured Image Credit: Ricardo Lima / MASTER / Getty


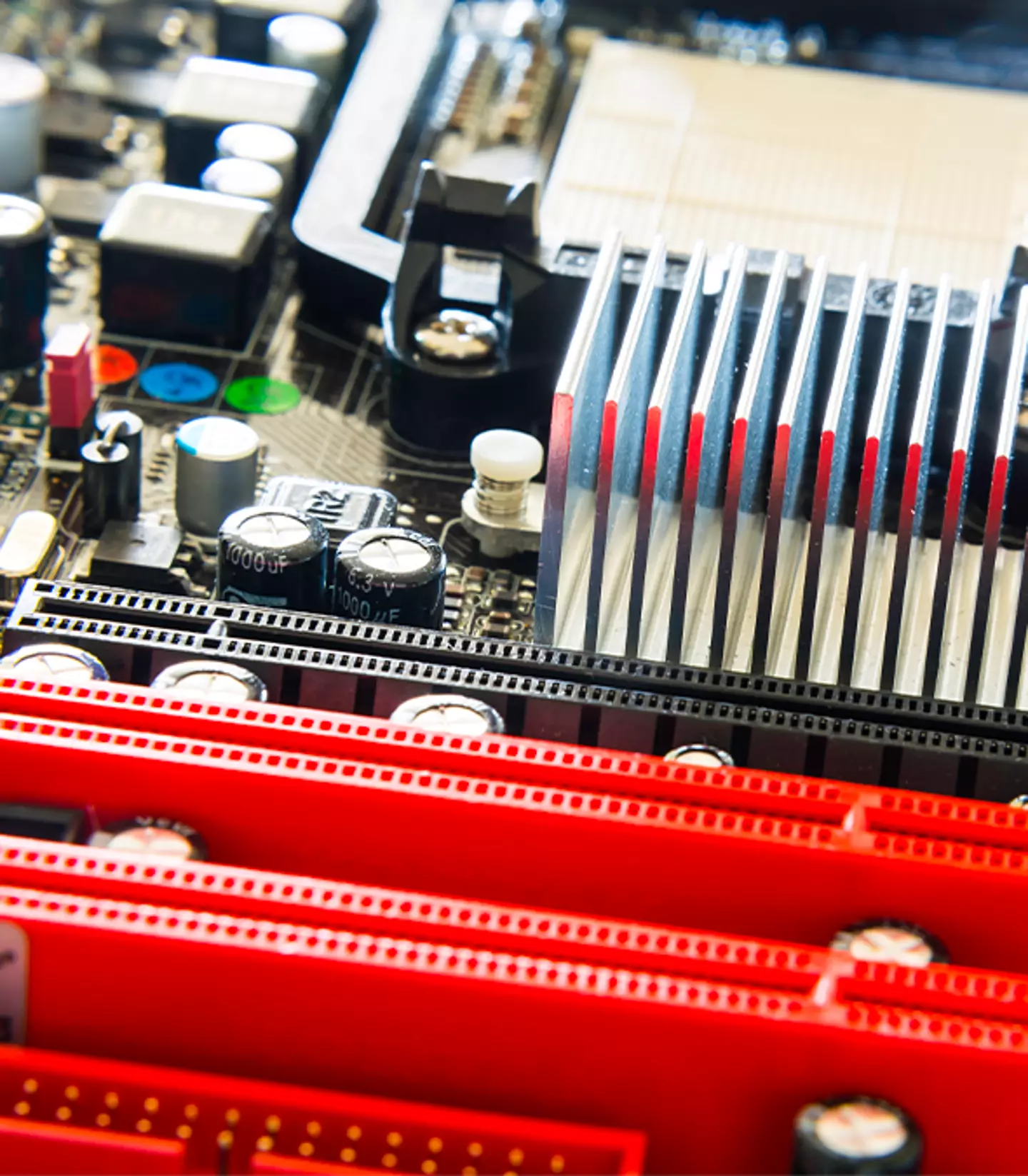
Imagine needing just a minute to charge your nearest devices. Sound too good to be true?
Well, researchers at the University of Colorado at Boulder may have just brought us a step closer to this reality.
Their breakthrough in understanding ion behaviour in supercapacitors could bring a whole new meaning to ‘super fast charging’.
The research could pave the way for a supercapacitor that can charge iPhones and laptops in just 60 seconds and electric vehicles (EV) in 10 minutes.
Supercapacitors were known to charge electronics lightning-fast however, the problem lies within their energy storage.
Traditional lithium-ion batteries can store significantly more energy, allowing for slower but longer use.


Onur Binay/Unsplash
Engineer and lead author of the study, Ankur Gupta, believes he and his team have found a key to overcoming this limitation – a technology that was known about but impossible to achieve.
The findings, published in the journal Proceedings of the National Academy of Sciences, focused on how charged particles (ions) move within supercapacitors. This movement is key to unlocking the long-awaited potential of supercapacitors for high-density energy storage.
Kirchoff’s Law, a defining principle in electrical current theory, establishes that voltage must move in specific loops.
‘The primary appeal of supercapacitors lies in their speed,’ read a press release from the university.
‘So how can we make their charging and release of energy faster? By the more efficient movement of ions.’
The unique behaviour of supercapacitors offers a way to bypass the limitations of Kirchoff’s Law and achieve much faster energy transfer.
‘That’s the leap of the work,’ said Gupta. ‘We found the missing link.’

risharp / Getty
The study lead explained that this could hold immense promise for ‘the future of the planet’.
While further research needs to be done before their findings can be worked into next-gen energy storage devices, it already concurs with previous studies from the University of Central Florida in 2016.
Their research focused on a flexible supercapacitor that could fully charge an iPhone in 60 seconds using advanced two-dimensional materials wrapped around nanometre-thick wires.
As a result, they achieved high energy and power densities as well as rapid charging and discharging cycles.
The best part is the compatible devices can withstand up to 30,000 charge cycles without degradation, far exceeding the 1,500 cycles seen within lithium-ion batteries.
Outside of personal electronics, Japanese automotive manufacturers have confirmed they’re all working on next-gen combustion engines which could change the future of transportation as we know it.

